Introduction: Autoimmune hemolytic anemia (AIHA) can occur as a primary disorder or as a secondary manifestation of an underlying autoimmune condition. The coexistence of anti-phospholipid syndrome (APS) and AIHA can be very complex and challenging to manage given the intertwining of the prothrombotic and hemolytic states. In this study, we explored the outcomes of underlying antiphospholipid syndrome in autoimmune hemolytic anemia hospitalizations.
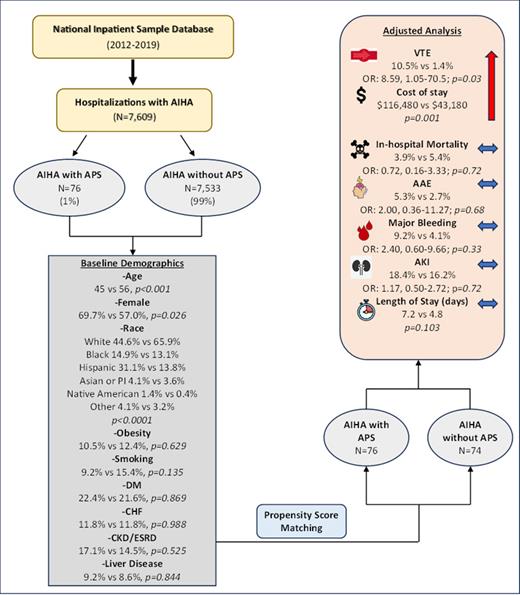
Method: The National Inpatient Sample (NIS) database was queried using the International Classification of Diseases (ICD) codes to identify hospitalizations for AIHA and then the data was subclassified into hospitalizations with and without APS. Demographics, comorbidities, and outcomes were identified using appropriate ICD 9/10 codes. Propensity score matched cohorts were generated for APS status and adjusted for age, race, sex, smoking, obesity, DM, CHF, CKD/ESRD, and liver disease.
Results: A total of 7,609 AIHA hospitalizations were included, with 76 patients having underlying APS and 7,533 did not have APS. Mean age was younger in the APS cohort and there were also more females, blacks and Hispanics compared to the non-APS cohort. Propensity score matching was used to generate two cohorts, adjusting for age, race, sex, and for co-morbidities including obesity, smoking, DM, CHF, CKD/ESRD and liver disease. The adjusted analysis showed an 8.59 times higher risk of developing venous thromboembolic events (VTE) in AIHA with APS as compared to those hospitalizations without APS (Odds ratio (OR): 8.59, CI: 1.05-70.5; p=0.03). There was also a statistically significant increase in mean hospitalization cost in the APS group (p=0.001). A trend towards more arterial athero-embolic events (AAE), major bleeding events, and AKI as well as longer length of stay was seen in hospitalizations with APS, but it did not reach statistical significance. No significant difference in in-hospital mortality was seen between the two groups. The results are summarized in the Figure 1.
Conclusion: APS confers additional risk to AIHA hospitalizations with significantly higher VTE events and added costs. Further studies should address the complex management of anticoagulation and prothrombotic risk in APS in the setting of active hemolytic anemia.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal